Studies have revealed that sleeping less than 5 hours each night is linked with a 74% increased risk of peripheral artery disease compared to sleeping 7-8 hours each night, suggesting this may be an effective method for decreasing peripheral artery disease risk. Thus, sleeping for at least 8 hours every night may help protect against peripheral artery disease risk.
Over 200 million individuals globally suffer from peripheral artery disease, in which leg arteries become blocked with plaque and restrict the blood flow, increasing risk for heart attack or stroke.
Sleep deprivation at night and frequent daytime napping has long been associated with an increased risk of coronary artery disease due to clogged arteries.
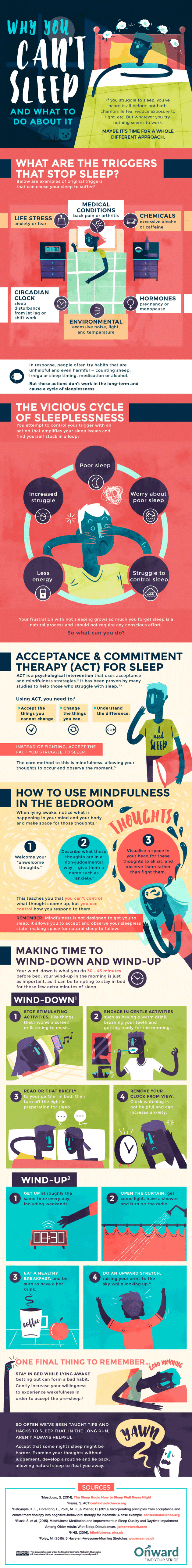
Sleep problems are one of the primary complaints among those living with peripheral artery disease, but data are lacking on how sleep habits impact this condition, vice versa; thus this study sought to uncover this correlation.
This study involved over 650,000 individuals and involved two stages. First, researchers evaluated how sleep duration and daytime napping related to peripheral artery disease risk.
In Part 2, researchers utilized genetic data to conduct naturally randomized controlled studies known as Mendelian randomization to examine causal relationships.
Observational analyses can be hindered by reverse causality; that is, it cannot be said with certainty whether sleep habits caused peripheral artery disease or vice versa. Mendelian randomization offers more accurate causal assessments.
Taken as a whole, short sleep provided the strongest evidence linking it to peripheral artery disease – both positively and negatively. An observational analysis involving 53,416 individuals concluded that sleeping less than five hours each night increased by almost double its risk when compared with sleeping seven to eight hours each night.
This result was confirmed through additional analyses conducted on 156,582 and 452,028 individuals, who both showed links between short sleep duration and an increase in peripheral artery disease risk, and short sleeping. Short sleeping was associated with increased risks associated with peripheral artery disease in causal studies while peripheral artery disease itself increased the likelihood of short sleeping episodes.
These results demonstrate that inadequate night-time rest may increase the risk of peripheral artery disease, while being diagnosed with PAD increases that risk as well.
Longer sleep was associated with a 24% higher risk of peripheral artery disease in an observational analysis conducted among 53,416 individuals who slept 8 hours or more every night than those sleeping between 7-8 hours per night.
This result was confirmed by two larger population analyses involving 156,582 and 452,028 people, although no causal associations between long sleep and peripheral artery disease could be established. Similar findings were seen for daytime napping: those engaging in this practice had an increased risk for peripheral artery disease by 32% over those who didn’t nap – though no causal links could be detected between napping in daytime hours and peripheral artery disease risk.
Studies must continue on the relationship between extended night-time sleep, napping during the daytime, and peripheral artery disease. Although observers found relationships, causality could not be proven conclusively.
Research must also focus on ways to interrupt the bidirectional relationship between short sleep and peripheral artery disease. Lifestyle changes that encourage individuals to get more restorative sleep – including being physically active – could reduce peripheral artery disease risk; for those already living with peripheral artery disease, optimizing pain management could provide them with better rest.